
Methods
Nasal nitrogen oxide measurement [nNO]
NO is produced by the epithelial cells of the airways for local immune defense. In healthy individuals, the NO concentration in the nose is between several 100 and >1000 ppb. If PCD is present, the concentration is often greatly reduced to a few ppb (the reasons are still unclear). Therefore, the measurement of nNO is very suitable as a screening method. However, since there are also PCD cases with normal nNO values, comprehensive diagnostics should be performed in cases of high clinical suspicion even with normal nNO values.
The technique of nasal NO measurement is age-dependent. Normally, the patient exhales continuously against a slight resistance (with the help of a mouthpiece) and a tube fixed in one nostril conducts the air from the nose to the measuring device.
Nasal Brushing
In order to study the beating of the cilia in the nose, we extract nasal epithelial cells by means of brushing. For this purpose, two small brushes are inserted into each nostril and cells are extracted from the inferior turbinates by means of a rotary motion.
The extraction is usually perceived by the patients as unpleasant to painful. However, the whole procedure takes only a few seconds and the pain is over as soon as the brushes are out again. If necessary, the removal can be facilitated by the use of a sedative. Local anesthetics (lidocaine or similar) should be avoided, as they can falsify the results.
High-speed video analysis (HSVM, HVMA)
The obtained cells are viewed under a light microscope (400x magnification) and a high-speed camera is used to record the cilia beat (at 300 frames/second). Special programs (“Cilialyzer”) then allow a detailed analysis of the cilia beat in slow motion (see video under PCD?->Basics). The beat pattern (movement, amplitude, coordination within a cell as well as between cells) and the beat frequency are assessed and.
Immunofluorescence (IF)
IF visualizes specific structural proteins of the cilia and, if necessary, shows their absence. This method is faster and less expensive than TEM and also allows the detection of certain defects that are not visible in TEM. It is in the process of establishing itself as an additional important method in PCD diagnostics.
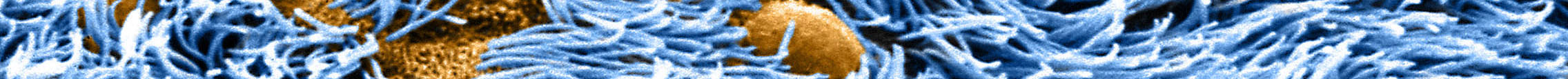
Transmission electron microscopy (TEM)
The examination of the ciliary ultrastructure by TEM has long been considered as «gold standard» of PCD diagnosis. Today, however, we know that several known PCD-causing mutations are associated with normal ultrastructure. Therefore, TEM today is primarily used as confirmation. The ciliary ultrastructure consists of nine double and two single central tubules (the so-called 9+2 structure, see figure under PCD?->Basics). The double tubules have outer and inner dynein arms, are connected to each other by a regulatory nexin-dynein complex and to the center by radial spokes. TEM analysis primarily allows to detect defects of the outer and inner dynein arms, disorganization of the tubules and disorder of the orientation of cilia. TEM analysis is time-consuming, cost-intensive, requires a lot of experience and the appropriate equipment. Therefore, we perform TEM only in selected cases.
Cell culture
The cells obtained from the nose by brushing often show abnormalities that are not due to the genetic defect, but rather originate from infections or the processing (so-called secondary defects). Culturing the harvested nasal cells at the air-liquid interface (air-liquid-interface) allows us to eliminate those secondary abnormalities and increases the number of usable cells (for HSVM, TEM and IF). The methodology is challenging, but we have been using it for quite some time with a high success rate (about 90%).
Genetic testing
Beginning of 2021, more than 50 genes had already been identified whose mutations can lead to PCD. Genetic analysis is becoming increasingly important and can already be used today as a stand-alone diagnostic method. However, analysis is not trivial and must be performed in a specialized center. Usually, "whole exome sequencing" is used for identification. In case of a hit, the mutation must then be confirmed by Sanger sequencing and a comparison with the parents. We cooperate with two centers for genetics (Human Genetics, Inselspital Bern and Genetics of the University Hospital Geneva).